Leaky gut, a condition scientifically referred to as increased intestinal permeability, has garnered significant attention due to its potential impact on various aspects of health, particularly its association with food intolerances involving IgG reactions to food proteins.
What is leaky gut and the connection with food intolerances?
The intestinal barrier serves as the body’s frontline defense, selectively permitting nutrients and substances to pass from the gut into the bloodstream while keeping harmful agents at bay. However, when the integrity of this barrier is compromised, as in the case of leaky gut, the intricate balance between absorption and protection is disrupted. This can lead to the passage of larger molecules, including food proteins, across the gut lining and into the bloodstream. In turn, the immune system may recognise these larger proteins as foreign invaders, triggering the production of IgG antibodies and potentially resulting in various symptoms and manifestations of food intolerance. Understanding the role of leaky gut in the context of food intolerances necessitates delving into the mechanisms that underlie this phenomenon and its implications for overall health and well-being.
Can food intolerances worsen leaky gut?
When an individual with leaky gut consumes foods to which they have IgG-mediated intolerances, a series of events can unfold that contribute to the worsening of both conditions. Here’s how this process works:
IgG Reactions and Inflammation:
In response to the consumption of specific foods, the immune system of a person with IgG sensitivities releases IgG antibodies. These antibodies target and bind to the offending food proteins, forming immune complexes. In the context of leaky gut, where the intestinal barrier is compromised, these immune complexes can more easily pass through the intestinal lining and enter the bloodstream.
Systemic Inflammation:
Once these immune complexes enter the bloodstream, they can trigger a systemic immune response and cause inflammation throughout the body. This inflammation can affect various organs and tissues, including the gut lining itself.
Impact on Leaky Gut:
The inflammation caused by the immune complexes can further compromise the integrity of the intestinal barrier. Inflammatory molecules can disrupt the tight junctions between the cells that make up the gut lining, making it even more permeable. This perpetuates the cycle of leaky gut, as the barrier’s function of selectively allowing nutrients and substances to pass through becomes increasingly impaired.
Delayed Healing:
Leaky gut is characterised by impaired tissue repair and healing within the intestines. The ongoing inflammation caused by both the leaky gut itself and the IgG reactions to food proteins can hinder the healing process. The constant influx of immune cells and inflammatory molecules to the gut lining can prevent the repair of damaged tissues, prolonging the leaky gut condition.
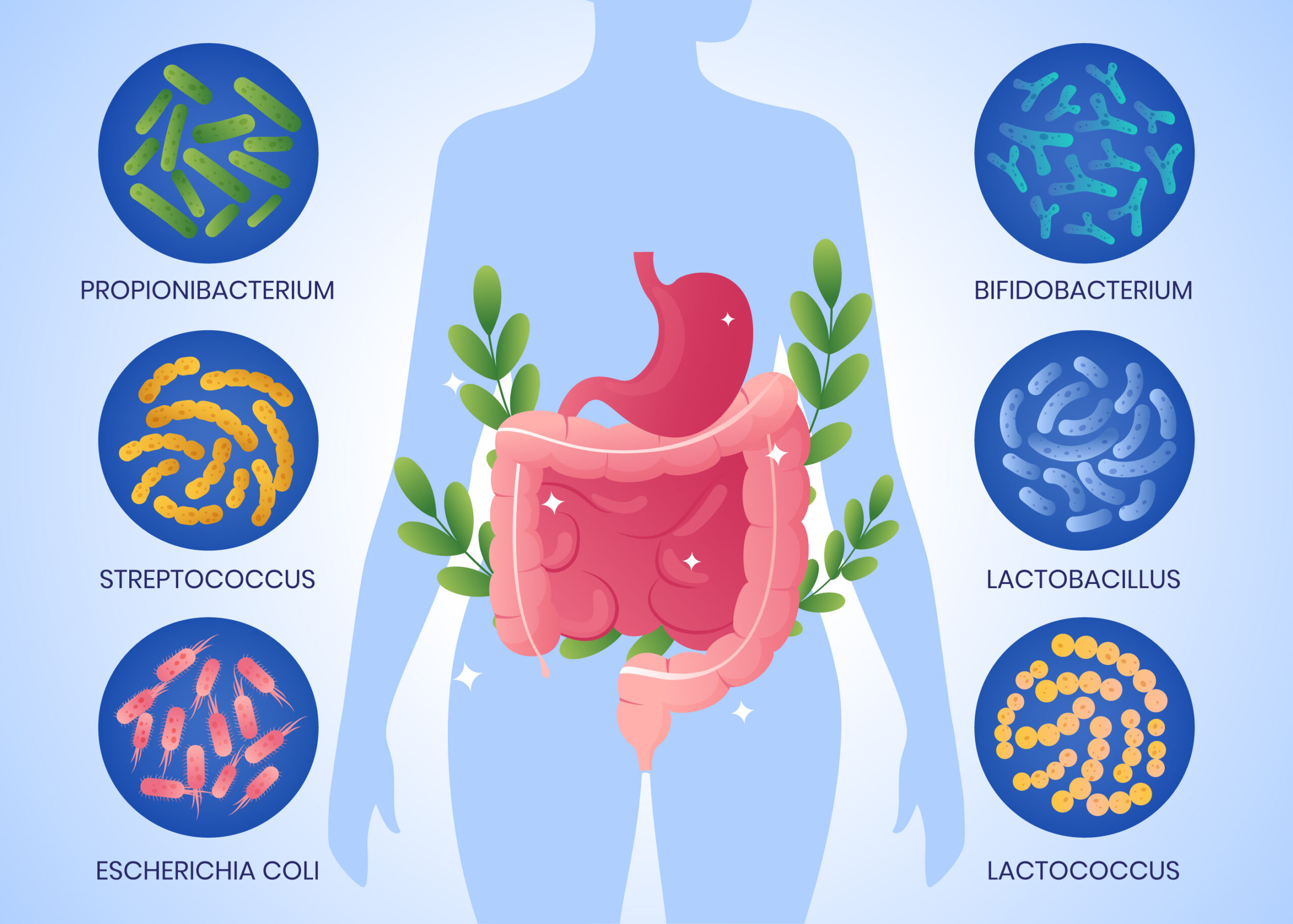
Microbiome Imbalance:
The gut microbiome, which plays a crucial role in gut health and immune function, can be adversely affected by both leaky gut and chronic inflammation. Dysbiosis (an imbalance in the gut microbial community) can develop, further contributing to inflammation and impaired gut barrier function.
Why your microbiota matters
Our In-House naturopath and microbiome specialist, Hannah, shares why your gut microbiome matters for restoring leaky gut, and why you shouldn’t ignore it.
Strong gut barrier
- Good gut bacteria, like Bifidobacteria species, Lactobacillus species and Faecalibacterum praustnizii play a crucial role in gut barrier health.
- Good bacteria protect us from leaky gut by producing ‘short chain fatty acids’ like butyrate.
- One of the most important functions of butyrate is its role in maintaining the health and integrity of the intestinal lining. It also helps to regulate the immune system and reduces inflammation in the gut, which is important for preventing and treating various gastrointestinal disorders.
- When the gut is permeable, food proteins can more easily access the blood stream, this is how IgG food intolerances develop.
Reduce or trigger inflammation
- Some bad bacteria that can overgrow in the microbiome (for example Citrobacter species, Escherichia coli) produce endotoxins called lipopolysaccharides. These can generate inflammation within the bowel, triggering leaky gut, as well as inflammation in the whole body. In this instance, removing food intolerances alone will not completely heal leaky gut, a holistic gut microbiome building protocol will help.
- On the other hand, beneficial bacteria which produce short chain fatty acids, dampen inflammation the the gut. In the case of butyrate, this has been shown to exert anti-infammatory activity in the whole body.
- Bacteria which trigger or reduce inflammation are directly protecting or feeding into a cycle of leaky gut.
Nutrient production and absorption
- Did you know your good bacteria are helping you to create nutrients like B vitamins (for energy) and vitamin K2 (healthy heart and bones)?
- Beneficial bacteria keep the pH of the bowel slightly acidic, which helps you to absorb minerals like iron, calcium and zinc.
- These nutrients are then used to maintain gut barrier health.
In summary, the relationship between IgG-mediated food intolerances and leaky gut creates a feedback loop of inflammation and compromised gut barrier function. The inflammation triggered by IgG reactions worsens the existing leaky gut, while the leaky gut, in turn, exacerbates the immune response to food proteins. This cycle can impede the healing process, prolonging the inflammation and preventing the gut from restoring its proper barrier function.
Addressing both IgG-mediated food intolerances and leaky gut through a comprehensive approach that includes dietary modifications, gut-healing protocols, can be crucial in breaking this cycle and restoring gut health.
How can I test my gut microbiome?
We are proud to offer a Practitioner Only Comprehensive Stool Flora Analysis. Hannah has been interpreting the gut microbiome for 6 years, so you won’t receive generic advice, but targeted treatments specifically for you. We are happy to assist you with accessing Practitioner Grade products to restore your gut.
Aside from a comprehensive look at bacteria, parasites, yeasts, worms, viruses and pathogens, this test also provides markers of inflammation, digestion, immune function, liver function and provides a holistic treatment plan.
For a discounted package including our most popular ImuPro Complete test, check out our Gut Health Package.